The New Nation
The 10th Amendment to the Constitution became the underpinning for the entire medical licensing system as powers not granted to the federal government, nor prohibited to the states, were to be reserved to the states or to the people.
Medical societies continued to provide the most common mechanism for medical regulation in the early republic but with varying success. North Carolina's first medical society collapsed within several years. New York enacted an elaborate system predicated upon county medical societies selecting examiners to screen prospective candidates for admission. In most instances, state legislatures looked to work in concert with medical societies as the mechanism for regulating the practice of medicine. Along the eastern seaboard, medical schools were seeking accommodations with medical societies. After the War of 1812, medical schools began to proliferate in the United States, particularly west of the Appalachians. Most were commercial, proprietary endeavors of noticeably poor quality.
Periodic epidemics exposed the limits of medical science as it stood in the first half of the 19th century. The 1832 cholera epidemic is instructive. Lacking an understanding of contagion theory and unaware of the existence of bacteria, physicians' treatments for patients often reflected the harsh remedies of the 'heroic' age of medicine, e.g., bloodletting and calomel, a mercury compound. The failure of traditional medicine's therapeutics opened the door to alternative treatment methodologies. These alterative schools of medicine attracted adherents and wide public support. This chaotic era of medicine contributed to the demise of most licensing laws in the United States beginning in the 1830s.
Therapeutics and the Rise of Sectarian Medicine
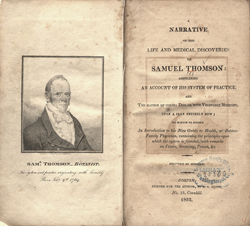 The Jacksonian era cult of the common man saw an explosion of complementary or alternative methods for medicine. Samuel Thomson developed a botanical-based medicine predicated upon the idea that the source of all disease stemmed from cold, with heat as the key therapeutic treatment, e.g., steam baths. His published works created a mass following in rural America that embraced the notion of reclaiming medicine from the hands of physicians. Samuel Hahnemann's homeopathic philosophy was built upon two concepts: the notion that "like cures like" and the law of infinitesimals. His drug therapies stemming from these principles resulted in administering drugs in such small doses as to have minimal effect; in effect, leaving nature to do the work of healing. The eclectic school of medicine comprised the other major "irregular" group of practitioners prior to the Civil War. They relied heavily upon botanical or herbal remedies; unlike Thomsonians, however, they advocated treatment guided by physicians rather than laymen. The most significant challenge to traditional medicine came later from Andrew Taylor Still and osteopathy. The success of osteopathic medicine is perhaps best attributed to its gradual incorporation of traditional medical theories and practices as the underlying science advanced, while retaining its distinctness in philosophy and in the practice of manipulation. All of these irregular practitioners were successful in establishing strong, viable challenges to traditional medicine. With the next wave of licensing laws starting in the last quarter of the 19th century, these groups gained legal protections for their practice.
The Jacksonian era cult of the common man saw an explosion of complementary or alternative methods for medicine. Samuel Thomson developed a botanical-based medicine predicated upon the idea that the source of all disease stemmed from cold, with heat as the key therapeutic treatment, e.g., steam baths. His published works created a mass following in rural America that embraced the notion of reclaiming medicine from the hands of physicians. Samuel Hahnemann's homeopathic philosophy was built upon two concepts: the notion that "like cures like" and the law of infinitesimals. His drug therapies stemming from these principles resulted in administering drugs in such small doses as to have minimal effect; in effect, leaving nature to do the work of healing. The eclectic school of medicine comprised the other major "irregular" group of practitioners prior to the Civil War. They relied heavily upon botanical or herbal remedies; unlike Thomsonians, however, they advocated treatment guided by physicians rather than laymen. The most significant challenge to traditional medicine came later from Andrew Taylor Still and osteopathy. The success of osteopathic medicine is perhaps best attributed to its gradual incorporation of traditional medical theories and practices as the underlying science advanced, while retaining its distinctness in philosophy and in the practice of manipulation. All of these irregular practitioners were successful in establishing strong, viable challenges to traditional medicine. With the next wave of licensing laws starting in the last quarter of the 19th century, these groups gained legal protections for their practice.
In retrospect, the rugged individualism and anti-regulatory climate of the Jacksonian Era, combined with democratization of medicine as espoused by the Thomsonians and others, led directly to the collapse of medical regulation in the first half of the 19th century. Nearly every state repealed its penalties for the unlicensed practice of medicine. Physicians protected their interests with organizations such as the American Medical Association (1847). The AMA Code of Ethics adopted in 1847 confronted the homeopathic challenge through its consultative clause prohibiting AMA members from case consultation with sectarian practitioners. This spawned a vigorous counterattack from the sectarians who waged successful legislative battles establishing separate licensing boards for homeopathic, eclectic (and later osteopathic) physicians.
The Return of Licensing Laws
The proliferation of poor quality medical schools threatened to saturate the field of medicine. With collapse of medical regulation in the 1830's, a medical license became a credential of limited utility. The public was uninterested in the sectarian debates among physicians and increasingly viewed credentials (whether a degree or license) as irrelevant as long as the diagnostics and therapeutics of medicine practice remained poor.
The 1861 onset of the Civil War represented different challenges. One challenge was identifying a qualified cadre of physicians to treat sick and wounded soldiers. Volunteer organizations such as the United States Sanitary Commission stepped in where the government faltered under the strain of sheer numbers of casualties.
The post-war reinstitution of a medical regulatory system in America can be traced to several factors. Most important was a change in public attitude. Once licensing had been equated with "power and privilege." Now it became identified with protecting the interests of the public health and independent professionals, both of which now seemed vulnerable in an emerging age of industrial titans like Rockefeller, Carnegie, etc. Large corporations seemed to threaten the idealized American vision of a nation driven by the economic engines of the yeoman farmer, artisan and small businessman. Recognizing the value of qualified physicians to help promote the public's health, not to mention the value of qualified engineers and architects, occupational licensing developed anew starting in the 1870s.
North Carolina was one of the first states to emerge out of this professional and regulatory dark age, even before the Civil War, with the establishment of a medical board in 1859. Texas adopted its medical licensing authority in 1873, Nevada in 1875, Alabama and California in 1876, Illinois in 1877, Minnesota in 1883, Colorado and Washington in 1881, New Mexico in 1882, Virginia in 1884 and Oklahoma in 1890. Nearly all states had established licensing boards and examinations by 1910.
On the western coast, California experienced a unique situation. The gold rush and a perceived "healthy climate" drew tens of thousands of newcomers. Multiple boards of examiners were established starting with medicine (1876) then Eclectic and Homeopathic boards in 1878. One of the most comprehensive efforts to curb the blatant excesses ongoing in medical education took place in Illinois. The Illinois' board introduced a "classification" system for medical schools that predated the work of the Association of American Medical Colleges and the AMA Council on Medical Education. The board's classifications soon became the de facto "authoritative" listing for all medical licensing boards.
Meanwhile, the United States Supreme Court upheld the authority of state medical boards to license and discipline physicians. The two seminal cases were Dent v. West Virginia in 1889 and Hawker v. New York in 1898.
The rebirth of medical licensing laws in late 19th century arose from multiple forces: professional aspirations for greater prestige; competing schools of medicine striving for recognition; a burgeoning number of medical schools; advances in medical science; and growing public awareness of (and perhaps impatience with) the ramifications of a purely laissez-faire economic system upon individual consumers.

